Blind To The Risk: 4 Ways To Avoid Blindness From Dermal Fillers
Dermal Filler complications are rare, but do present a real risk. In this article, Harley Academy experts explain blindness induced by injectable treatments and how to avoid it.
In this article we look at one of the most serious dermal filler complications: blindness. You’ll learn what causes blindness when injecting dermal fillers, how to avoid it and what training can make you a safer aesthetics practitioner.

Current statistics for dermal filler blindness
The global injectables market is predicted to more than double over the next decade according to a 2016 article in Dermatology Times. One reason for this increasing popularity is that injectables are seen as ‘non-invasive’, alluding to the minimal disruption to tissue when performed competently.
However, whilst the popularity of dermal filler treatments is enjoying an almost exponential increase, so are reports of attendant complications. Although rare, complications from dermal fillers can be devastating.
The most serious complications are vascular. Vascular occlusions can lead to necrosis (tissue death), scarring and, even more seriously, blindness. Indeed, dermal fillers have already led to 98 reported cases of blindness (Beleznay et al, 2015).
In a recent literature review (Beleznay et al, 2015), Hyaluronic Acid (HA, also known under brand names Restylane®, Hydrafill®, Hylaform® and Juvederm®) was the second most common type of filler associated with ocular complications, after autologous fat injections. HA is the most frequently used soft tissue filler in cosmetic practice.
Out of 98 cases of vision complications from dermal fillers, 65 led to unilateral vision loss, and only two cases of vision loss were reversible.
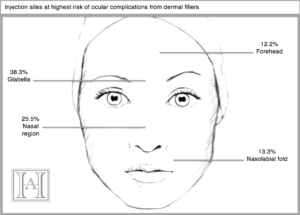
Injection sites at highest risk were glabella, nasal region, forehead and nasolabial fold.
How can dermal filler injections induce blindness?
The basic mechanism of filler induced blindness is fairly simple: central retinal artery occlusion.
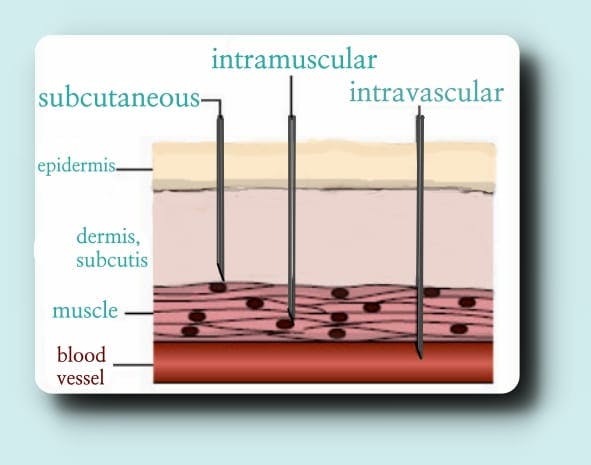
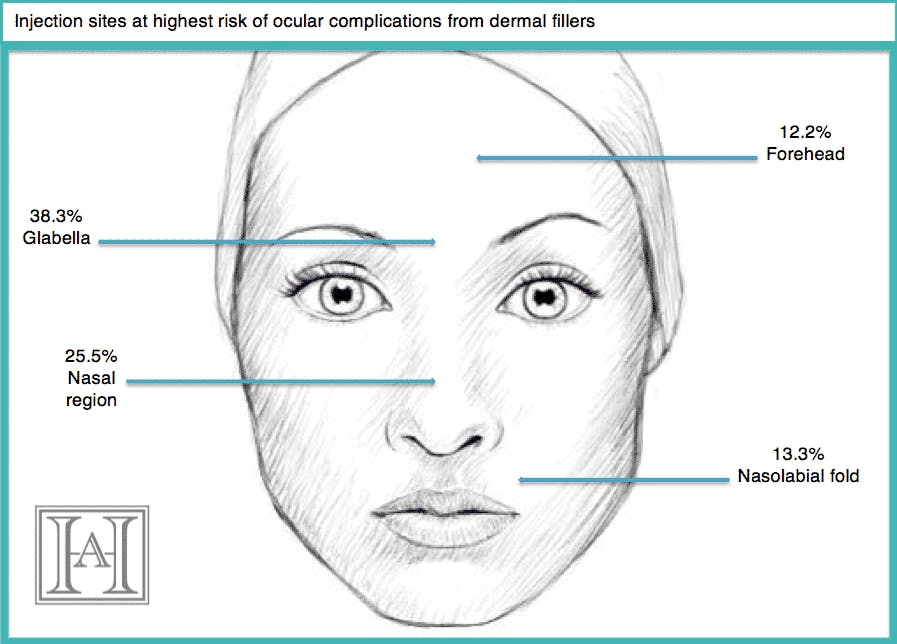
If the tip of the needle penetrates the vessel, leading to an intravascular injection, and too much pressure is applied to the plunger when injecting, the arterial pressure can be overwhelmed and retrograde movement of HA into the more proximal arterial network can occur.
Eventual embolisation into the central retinal artery will deprive the retina of oxygen and lead to blindness.
How to avoid causing blindness with dermal fillers
“Soft tissue fillers are used for multiple cosmetic and therapeutic indications. Adequate clinician training in the use of these agents is essential for the prevention of adverse events.” – Carruthers et al. (2015), Injectable soft tissue fillers: Overview of clinical use
1. The only way to avoid arteries is to know where they are
It may seem obvious, but all clinicians delivering dermal filler injections must have an in-depth, working knowledge of vascular anatomy.
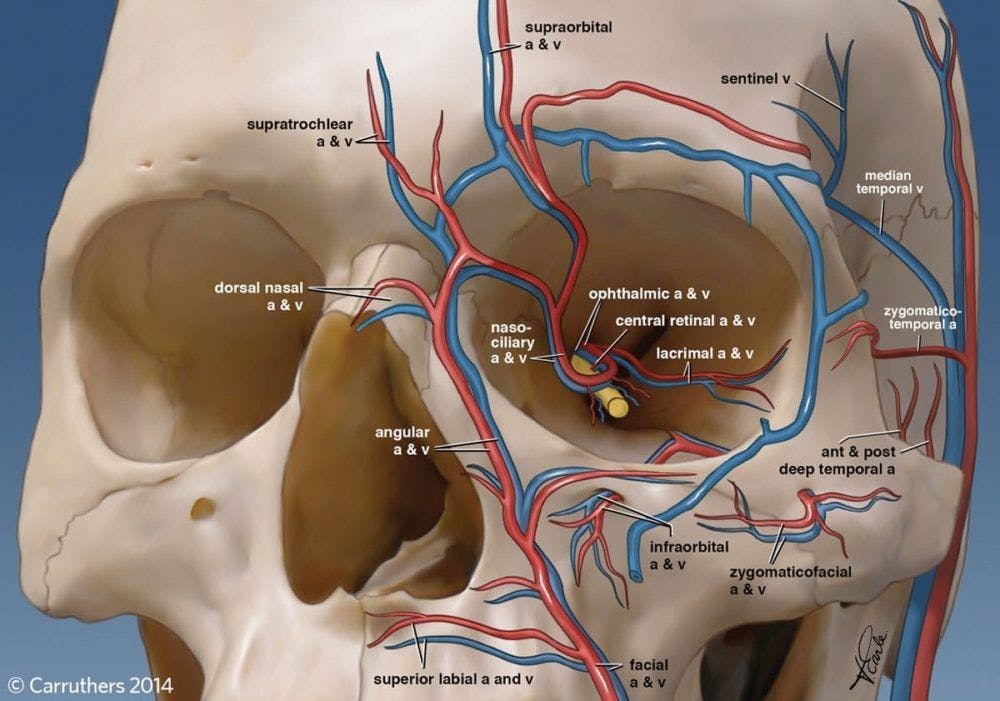
In their latest guidelines on qualification requirements for delivery of non-invasive cosmetic procedures, Health Education England (HEE) recommend that courses teaching injectables such as Botulinum Toxin and dermal fillers offer 50% theoretical training. This should, of course, include facial anatomy.
In their latest guidelines on qualification requirements for delivery of non-invasive cosmetic procedures, Health Education England (HEE) recommend that courses teaching injectables such as Botulinum Toxin and dermal fillers offer 50% theoretical training. This should, of course, include facial anatomy.
One of the changes made in Part Two of HEE’s 2016 guidelines was to raise the level of qualification requirements for temporary dermal fillers, so that no treatments are able to be delivered until practitioners have successfully completed a Level 7 Qualification (postgraduate level), at which point they would only be able to practise under clinical oversight
2. Inject slowly and incrementally
In many cases of retinal avascular necrosis, filler was injected with too much pressure.
3. Inject to the correct depth and plane, taking into account the relevant anatomy of the skin, muscle, vessels and fascia.
4. Even with all of the above, no procedure is immune to error
You must have a management strategy in place, and be able to refer the patient immediately to an ophthalmologist within the limited window of opportunity to reverse the effect – after complete central retinal artery occlusion, the retinal survival time is 60-90 minutes.
Although a quick intra-occular injection of hyaluronidase has been successful in dissolving the filler and preventing permanent blindness, there’s no agreed method for reversing central retinal artery occlusion from fillers. Some advanced courses will cover central retinal artery occlusion, and advise using the latest medical knowledge.
Awareness of dermal filler risks
At the time of writing, Googling ‘risks of dermal fillers’ brings up the following NHS summary:
‘General risks of dermal fillers include: problems such as rashes, swelling, itching and bruising. The filler can move away from the intended treatment area over time. You may have an immediate allergic reaction to the filler, which can lead to anaphylaxis.’ – Non-surgical cosmetic procedures – NHS Choices
So, with only superficial research, one might be led to think that beyond minor risks, fillers are safe — regardless of who is injecting. Clearly, however, patient outcomes can be much worse.
Awareness of the risks should not only be more publicly available, but also embedded in the regulatory systems of the cosmetics industry. With no formal qualifications or medical training requirement for delivery of dermal fillers, it is not surprising that some have denounced treatments like dermal fillers as a “crisis waiting to happen” (Keogh report, 2013).
‘Anybody, anywhere, anytime can give a filler to anybody else, and that is bizarre.’ – Sir Bruce Keogh, NHS Medical Director
Ultimately, only with proper medical training can the far more potentially devastating risks be minimised in the first place. Are you prepared for such a crisis?
Harley Academy Training in Dermal Fillers
From our entry-level Foundation Training and Core Training in Botox & Dermal Fillers, to our industry-leading Level 7 Diploma in Botox & Dermal Fillers, and Injectables Masterclasses, find out more about our toxin and filler training courses.
You can also enjoy self-paced home-learning with our dedicated Preventing and Managing Dermal Filler Complications eLearning, which is available to purchase separately.
Last fact-checked: 26 January 2023
References
Beleznay, K.,Carruthers, J. D. A.,Humphrey, S., Jones, D., (2015) Avoiding and Treating Blindness From Fillers: A Review of World Literature. Dermatologic Surgery: October 2015 – Volume 41 – Issue 10 – p 1097–1117 doi: 10.1097/DSS.0000000000000486
Carruthers, A., Carruthers, J., Humphrey, S., (2015) Injecting soft tissue fillers: Overview of clinical use. ©2016 UpToDate
Further reading
Vascular Compromise from Soft Tissue Augmentation: Experience with 12 Cases and Recommendations for Optimal Outcomes Beleznay et al (2014)
HEE guidelines 2016: A Brief Summary