What Are Exosomes? A Guide for Aesthetic Practitioners
Exosomes have quietly become one of the most talked-about additions to the aesthetic practitioner’s toolkit in recent years. They’ve gained traction with clinicians seeking the next edge, as they’re new yet still grounded in biology.
You may have already seen them on your social feeds, in supplier newsletters, or mentioned at conferences. The buzz is there, but so are the questions. And not just the usual: what are they, do they work, and should I offer them?
There's a more complex conversation unfolding around the exosomes hype. Injectors are intrigued by the mix of science, marketing, clinical curiosity and, understandably, scepticism.
So, let's unpack this in our aesthetic practitioner’s guide to exosomes…

What are exosomes?
At their simplest, exosomes are tiny extracellular vesicles, nano-sized bubbles, that act like messengers between cells. They’re naturally produced by almost all cells in the body and are packed with a cargo of proteins, lipids, RNAs and various signalling molecules.
Think of them as parcels sent from one cell to another. They help regulate everything from inflammation to cell regeneration. In many ways, they reflect the status of their parent cell, passing on that "information" to nearby cells.
In the context of facial aesthetics, it’s the regenerative potential that catches most people’s attention.
These vesicles, especially those derived from stem cells, appear to carry pro-healing, anti-inflammatory and tissue-supportive instructions. The idea is that, by introducing them to the skin, usually in a topical format post-procedure, they can enhance the healing cascade and optimise outcomes.
That’s the theory, but substantive, peer-reviewed data on the practical outcomes is still a developing space.
Why are exosomes so controversial?
Exosomes have arrived in aesthetics during a period where the industry is increasingly scrutinised, especially by the media, and by patients themselves. Safety, transparency, and ethical sourcing are all under the spotlight.
Some exosome products claim impressive benefits in their marketing, but come with little published clinical data. That immediately, and quite rightly, raises eyebrows.
Concern over exosomes ‘causing’ cancer
One particular concern that has fueled controversy among aesthetic medicine practitioners is whether exosomes can cause cancer. They are not carcinogens, however, as biological messengers, they can influence the behaviour of cells, which is where this worry comes from.
Exosomes carry signalling molecules that can tell other cells what to do: grow, divide, repair, reduce inflammation, etc. This, therefore, begs the question, what happens if these instructions are received by a cell which is already damaged, pre-cancerous or “on the edge”?
This is still very much theoretical in the aesthetic context, but it’s thought that exosomes could potentially promote an environment that supports cancer cell survival or proliferation. If the exosomes themselves carry growth-promoting signals - which many do, especially those from mesenchymal stem cells - this is an even more valid concern.
What does the research say?
There is research showing that tumour cells release their own cancer-derived exosomes to support tumour growth, metastasis and immune evasion. Zheng et al. (2022) on miR‑100/143‑rich MSC exosomes suppressing colorectal cancer (PubMed ID 36152993) is one such study.
It’s important to make the distinction as to them being ‘cancer-derived’ to differentiate them from the therapeutic exosomes used in aesthetics.
Conversely, some studies have suggested that MSC-derived exosomes might actually suppress tumour activity in certain contexts. One of these is Lee et al. (2013) on miR‑16‑mediated VEGF suppression in breast cancer (PubMed ID 24391924).
The data is mixed and highly context-dependent. What’s lacking is solid, peer-reviewed research into long-term safety of exogenous exosome use in healthy humans, especially in repeated or systemic applications.
In aesthetic medicine, where exosomes are most often applied topically post-procedure, the systemic exposure is likely low. But we don’t yet have definitive long-term safety data to say with certainty that there’s zero risk, especially in patients with undiagnosed malignancies.
Outside of this, there’s also the issue of where exosomes come from, which further explains much of the controversy’s origins.

What are exosomes made of?
Most exosomes used in facial aesthetics in North America and South East Asia are derived from human mesenchymal stem cells (MSCs). In the UK and Europe, however, these are banned so most sources are plant or animal derived.
Broadly speaking, exosomes contain a mix of nucleic acids, such as microRNAs, alongside proteins, lipids and metabolites. The exact composition varies depending on the source of the parent cell and how the exosomes were isolated.
For example, exosomes derived from MSCs tend to contain anti-inflammatory and regenerative molecules. But this depends heavily on culture conditions, harvesting techniques, and purification methods.
Exosomes are not a uniform product, which can make them challenging. It also makes quality control particularly important. You can’t always assume one exosome serum is the same as another.
Where are these stem cells sourced from?
The MSCs used in exosomes are most commonly from sources such as umbilical cord tissue or adipose tissue.
As umbilical cords are considered medical waste, these cells can be ethically donated with proper consent. Whereas, adipose tissue is often donated, following rigorous screening and consent, from patients who’ve undergone cosmetic surgery. This includes liposuction fat or surgical tissue discarded following procedures such as tummy tucks or breast reductions.
There can be discomfort when patients learn that exosomes are derived from human cells, particularly in relation to umbillical cords. It also puts aspects such as ethics, donor screening, cell banking standards, and even import laws, under the spotlight.
The plant and animal derived exosomes in the UK and Europe come from a number of sources. These range from bovine colostrum to stem cells from the umbilical cords of red deer. Although there are likely to be fewer ethical concerns with these, it’s still important to inform your patient where they come from.
How are these products regulated in the UK?
As we already know, the UK doesn’t have a great reputation for its aesthetics regulation in any capacity. Currently, exosomes exist in something of a grey zone. They're not classified as medicines, but they’re not fully regulated in the way medical devices are, either.
This ambiguity leaves a gap which some manufacturers fill with ambitious claims and glossy marketing. Others take a more cautious, research-led approach.
Clinicians, caught in the middle, are left trying to navigate both sides, which can be a source of frustration.
What are the benefits of using exosomes?
When used correctly, and sourced responsibly, exosomes can offer a number of potential benefits. Most often in facial aesthetics, they’re used as a topical, regenerative skin booster alongside collagen induction procedures such as microneedling, laser resurfacing, radiofrequency or PRP.
Harley Academy Cosmetic Dermatology Course mentors can discuss the use of exosomes after various skin treatments, during your practical training. Feel free to ask them any questions!
The main benefits attributed to exosomes include:
- Reducing inflammation
- Speeding up skin healing
- Improving skin texture and tone
- Supporting collagen production
- Reducing downtime following aesthetic procedures.
Patients often report skin feeling calmer and less irritated, with redness settling more quickly.
Due to their anti-inflammatory properties, improvements in chronic conditions such as systemic lupus erythematosus, psoriasis and atopic dermatitis, from exosome treatment may be possible. This is an area where much more research is needed, however.
There’s also anecdotal feedback suggesting that overall aesthetic results are enhanced, though how much of that is placebo is hard to say without stronger data.
Given how much media hype there is around right now, a word of caution is required when talking to patients about what type of results they’re likely to see.
The language used to describe exosomes in marketing materials and press coverage - "stem cell-derived", "cell signalling", "cutting-edge" - can set unrealistic expectations. It can mislead patients into believing they’ll see dramatic outcomes, which can be a tricky dynamic to manage, particularly when results are subtle or cumulative.
Exosomes aren’t miracle workers, but they can be valuable adjuncts, so ensure you manage your patients’ expectations candidly.
Downsides include lack of regulation, long-term effects and cost
We can’t look at the positives of exosome treatment without also exploring the negatives. These boil down to:
- Lack of regulation
- Cost
- Not enough robust safety data on long-term effects.
First up in this respect is the lack of regulation. It leaves room for poor-quality products and misleading claims, which can erode trust from both aesthetic practitioners and patients.
Next is the cost. Exosome serums are expensive, sometimes prohibitively so, when it comes to clinical products. That cost has to be absorbed either by you, or passed on to the patient, which isn't always viable for lower-ticket treatments. This can, in turn, create pressure to “upsell” their use, even when benefits may be marginal.
Some mainstream skincare brands have started to introduce exosome serums to their ranges. For example, The Inkey List launched a plant-based Exosome Hydro Glow Complex serum in April 2025. Undoubtedly, as they grow in popularity, other brands - both clinical and ‘high street’ - will start to do the same, which usually brings the price down.
Lastly, but incredibly importantly, is the broader concern about long-term effects, or, more specifically, the lack of robust safety data on the long-term, repeated use of exosomes. While they appear to be well tolerated, these are powerful biological agents so it’s wise to proceed slowly and remain cautious.
As we’ve already explained, the cancerous considerations are a significant sticking point for many clinicians. However, this information does require contextualisation.
How do you use exosomes as an aesthetic practitioner?
Right now, aesthetic practitioners who offer exosomes generally apply them topically after a skin-disrupting procedure. The idea is that the microchannels created during microneedling or fractional treatments allow for deeper penetration and encourage uptake.
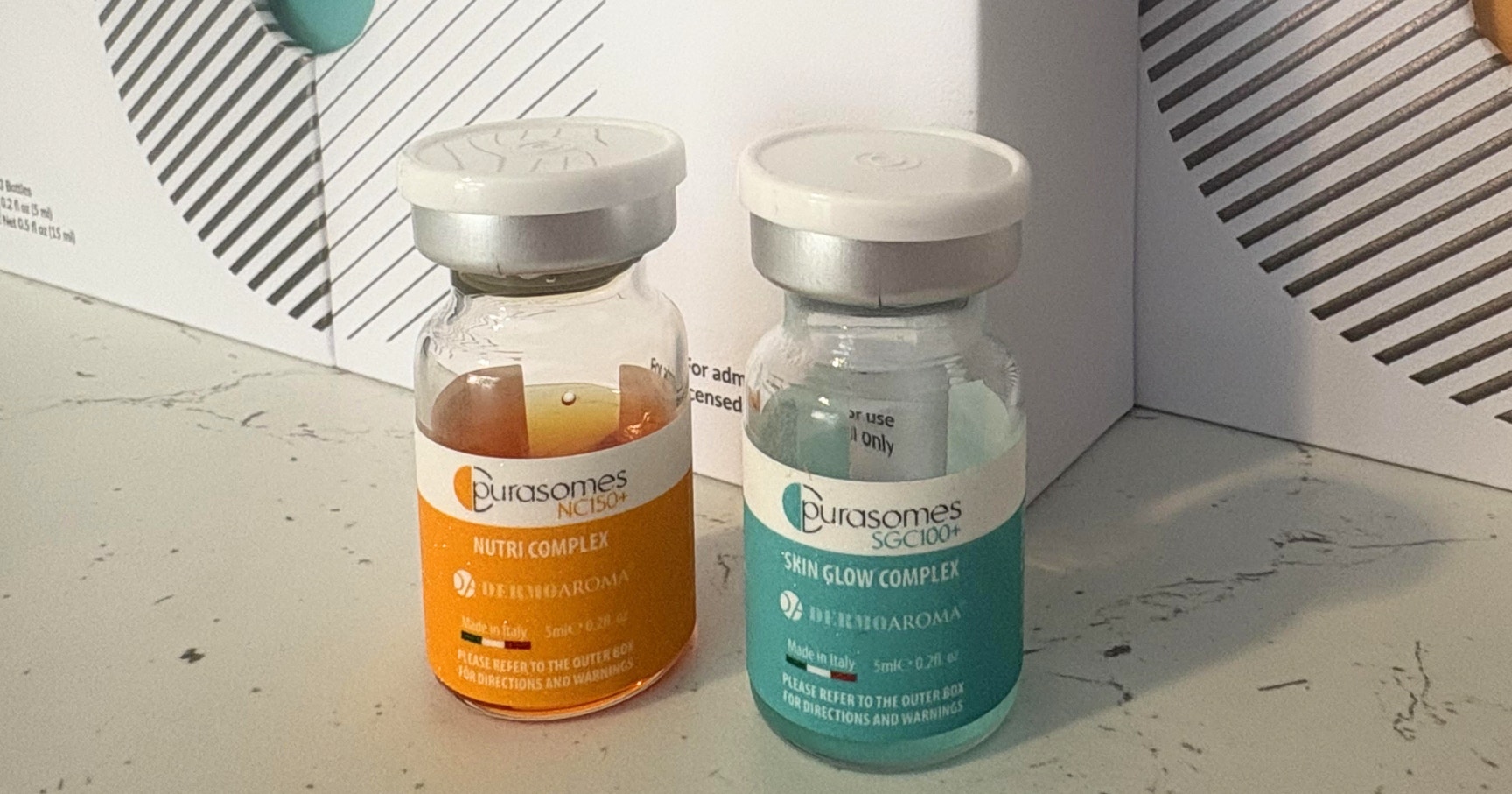
Some serums are designed specifically for this pairing. They usually come in small sterile vials and are used immediately after opening. You might also refrigerate or freeze them, depending on the formulation.
Protocols vary, but a typical approach tends to involve 3–5 sessions spaced 2–4 weeks apart, often combined with other treatment modalities. Results are usually gradual, so it’s important to set expectations accordingly, especially where patients are used to procedures that deliver a more ‘instant’ effect, such as dermal fillers.
Marketing them well, without overpromising, takes a bit of finesse. They’re a nice "add-on", but for many patients, the science behind them needs simplifying. Focus on recovery, skin support, and boosting results—not “miracle” outcomes.
Can exosomes be injected?
Technically, exosomes can be injected but in many countries, injecting exosomes would classify them as a medicinal product—requiring clinical trials, regulatory approval, and much tighter controls. That’s not something most aesthetic suppliers have, which means injecting them could carry legal and professional risk.
In the UK, the general consensus is that topical use is the safest and most compliant route. It may be tempting to use a mesotherapy-style approach, but unless you're absolutely certain of a product's regulatory status, it’s best avoided. There are currently no products in the UK that have been improved for injectable use.
Aside from the legal side, there’s not enough evidence yet to support injectable use. It’s simply not been studied thoroughly. In our industry, patient safety should always come first, so “just because you can” isn’t a strong enough justification.
What to look for in an exosome product
A good, topical exosome product should ideally be cell-free, so that it’s just the vesicles, no cellular material. It should also be sterile and free from contaminants such as endotoxins. These elements aren't always guaranteed, especially with online suppliers.
Doing your due diligence is critical when it comes to choosing an exosome product. There are some anecdotal reports of inconsistent results from exosomes, but these could potentially stem from variable product quality.
If you’re feeling uncertain about exosomes, that’s probably a good thing. It means you’re asking the right questions.
They’re promising, but not without caveats, and like many things in aesthetic medicine, their true value lies in how thoughtfully they’re integrated.
If you're considering them, start small. Trial with trusted suppliers, ensure your patients are fully informed and properly consented, then observe them closely. Collect feedback. You should also keep an eye on the evolving research.
We currently do not offer exosomes at The Academy Clinic, nor do we offer any dedicated exosomes training. You can, however, book in for exosome treatments at STORY Clinics, our boutique aesthetics clinics in London (Marylebone) and Nottingham (Southwell).
For now, exosomes courses are usually manufacturer-led. However, we keep our aesthetics training and treatment menus under review based on the latest evidence. We’re also happy to answer any questions you may have about using exosomes in conjunction with treatments such as microneedling, during our Cosmetic Dermatology Course sessions.
Hopefully, you’re feeling more informed about exosomes now. Let us know over on the Harley Academy Instagram account whether you’re excited about this new innovation!
All information correct at time of publication
Download our full prospectus
Browse all our injectables, dermal fillers and cosmetic dermatology courses in one document
By submitting this form, you agree to receive marketing about our products, events, promotions and exclusive content. Consent is not a condition of purchase, and no purchase is necessary. Message frequency varies. View our Privacy Policy and Terms & Conditions
Attend our FREE open evening
If you're not sure which course is right for you, let us help
Join us online or in-person at our free open evening to learn more
Our Partners













STAY INFORMED
Sign up to receive industry news, careers advice, special offers and information on Harley Academy courses and services


