Ptosis or Botulism: What Lid Droop After Botox Can Mean

Did you know that lid droop is a sign of botulism? A UK outbreak of botulism has been reported in the North East, linked to potentially fake ‘botox’, bringing this to the fore.
County Durham has seen 28 people present to the NHS with signs of botulism, weeks after toxin treatment. At least ten of these have required treatment, according to local newspaper, The Chronicle.
These cases, concentrated around Durham and Darlington, represent unprecedented demand for botulism treatment. For perspective, there were a total of six cases recorded in 2023-2024 across the whole of England.
The NHS describes botulism as ‘a rare but life-threatening condition caused by toxins produced by Clostridium botulinum bacteria’.
If you use an established, FDA-approved neurotoxin, with the appropriate safety marks, from a reputable source, you shouldn’t encounter this issue. It’s extremely rare and the limited cases usually involve counterfeit botox.
However, it’s worth every aesthetic practitioner educating themselves on how botulism symptoms present. In particular, ‘droopy eyelids’, which may be misread as ptosis.

An example of eyelid ptosis, where only the left eye shows droopiness
Allergan Aesthetics suspects counterfeit botox was used
In a press statement about this UK case, AbbVie company, Allergan Aesthetics - the maker of Botox - advised:
"Allergan Aesthetics is aware of recent reports of suspected botulism in patients in County Durham and Darlington, who received injections of a product, being referred to as ‘botox’.
"Investigations are ongoing, and Allergan Aesthetics is working with the local authorities. Allergan Aesthetics suspects that the product administered is counterfeit, further underpinning the importance of ensuring you are acquiring a genuine product through reputable and trusted channels.
"Allergan Aesthetics’ priority is the health and safety of patients and all reports of counterfeit product are thoroughly investigated by our team and in conjunction with law enforcement and regulatory authorities."
UKHSA, an executive agency, sponsored by the Department of Health and Social Care, is working closely with the council on this, too.
Update: On 18th July 2025, a warning was issued by UKHSA, which noted this situation had resulted in 38 cases of botulism. These were all related to the use of a fake botulinum toxin product injected by a non-medic, who has now apologised.
Forehead “frozen” within two hours of treatment
Additional, more recent, reports confirm the likelihood that these injections not only used fake Botox products. It seems they were also administered by inappropriately, or untrained injectors without a medical background, in unsuitable premises. The upper face treatments cost those affected around £100 for three areas. This pricing is unusually low as ‘three areas’ even at the cheaper end of the scale would usually be no less than £150 in this region.
An affected patient also ‘won’ a round of treatment in a competition. This was despite such giveaways and competitions being illegal due to Botox being a prescription medication.
One of the affected patients told the BBC of her symptoms, following treatment with what has been identified as illegal, fake Botox. The 37 year old advised that her forehead became “frozen” within two hours of having the upper face treatment. This rapid onset was the first red flag. Although there are regulated neurotoxins marketed as being ‘rapid onset’, such as Alluzience and Relfydess, Botox - which the toxin provided was said to be - is not one of these.
Next, her throat began to close up, one of her eyes swelled shut and one side of her face began to droop, within days of her treatment. She further noted being unable to smile, struggling to eat or swallow, feeling exhausted and desperately sleepy.
After being treated with an anti-toxin, made from horse blood, at the University Hospital of North Durham, an internal memo reportedly showed concern over the potential for more cases. The hospital has reportedly ‘exhausted’ all local stock of the anti-toxin, and is awaiting deliveries of 10 more batches from London.
A dedicated incident team has been set up and any concerned patients in the area are encouraged to get in touch.
The MHRA has now announced an investigation into these cases, following prompts from the BBC.
First UK cases following larger outbreaks in America
The cases centred in County Durham appear to be the first linked to aesthetic treatments in the UK. However, there have been a number of instances where this has been reported across the USA in the past few years. The Center for Disease Control advised that these were caused by ‘counterfeit products, products from unverified sources, or from individuals who were not following jurisdictional requirements.’
Always use a reputable supplier for your aesthetic medicine products
We’ve already written about this in depth, and urge you to read our previous article on How to Spot Fake Botox Products.
If you take the following steps, it’s highly unlikely that you’ll be at risk of patients developing botulism from neuromodulation:
- Only use authentic, reputable neurotoxin products
- Your toxin brand of choice should have passed all the relevant regulatory requirements for your country, such as gaining FDA approval or the UK Conformity Assessed mark (since Brexit, the CE mark is no longer recognised in the UK)
- Only purchase from the manufacturer or one of its authorised distributors
- Ensure the pharmacy you use clearly displays its Registered Pharmacy mark and number; you can look this up to check its authenticity
- Store and use your toxin as per the manufacturer’s guidelines.
That said, it’s still important for aesthetic practitioners to understand the signs of botulism.
Botulism symptoms aesthetic practitioners should know
The NHS advises that botulism symptoms vary depending on the exact type of botulism, and can present anything from a few hours to ‘several days’ after exposure.
NHS.uk states that some people ‘initially have symptoms such as feeling sick, vomiting, stomach cramps, diarrhoea or constipation.
‘Without treatment, botulism eventually causes paralysis that spreads down the body from the head to the legs.’
It advises that symptoms can include:
- Drooping eyelids
- Blurred or double vision
- Facial muscle weakness
- Difficulty swallowing (dysphagia)
- Slurred speech
- Breathing difficulties.
Whilst many of these will be easy to spot, how can you tell ‘drooping eyelids’ from lid ptosis? Let’s explore…
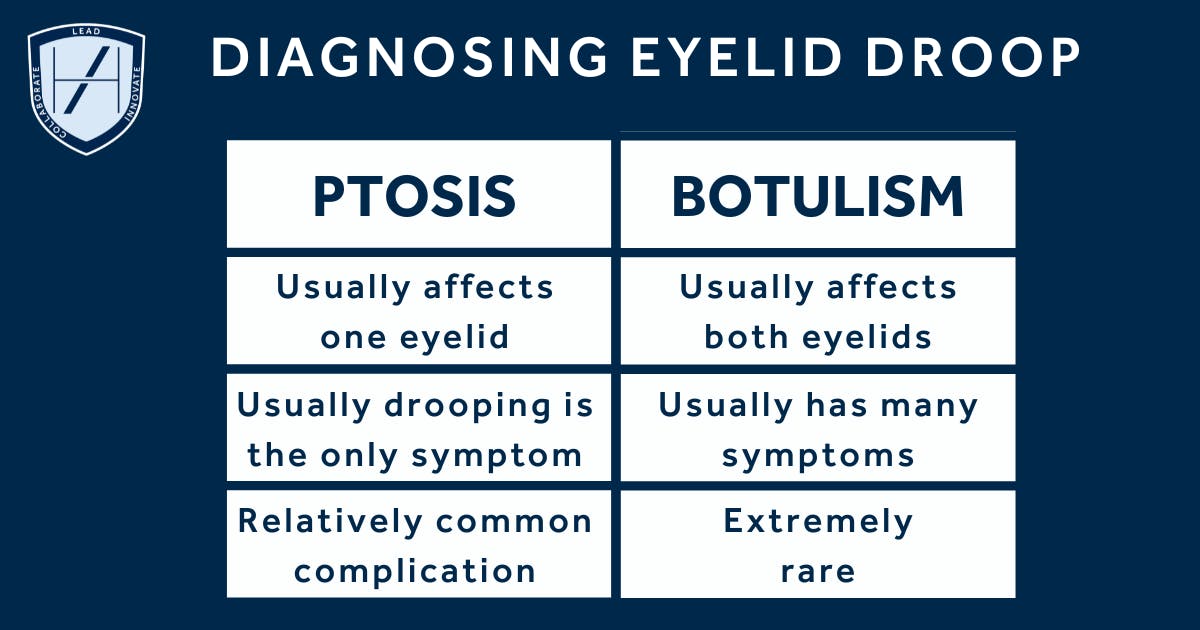
How to tell if droopy eyelids are ptosis or botulism
Droopy eyelids are a known complication after botulinum toxin treatment. But they’re also one of the early signs of something much more serious: botulism. Thankfully, the latter is extremely rare in aesthetic medicine.
If you’ve followed all the steps we’ve already outlined - using a reputable product, obtained from a reliable source, stored correctly - the chance of any drooping being botulism is extremely low. If your patient has no other botulism-related symptoms, any drop is likely ptosis.
This ptosis can be managed with eye drops and/or re-treatment, in many cases. It may also self-resolve without intervention over a period of weeks to months. This depends on the degree of severity.
In contrast, botulism is a systemic neurotoxic condition that doesn’t just affect one facial muscle. It begins subtly but progresses fast. Double vision, dry mouth, difficulty swallowing, generalised muscle weakness. In severe cases, respiratory failure. These are red flags.
Botulism tends to show bilateral ptosis, where both eyelids are drooping, whereas ptosis generally only affects one side. This droop may not always be dramatic at first, but it should be enough to notice that something’s wrong. In botulism, it rarely comes alone, so ask your patients if they’re experiencing any other symptoms.
Can they still blink normally? Is vision affected or just eyelid heaviness? Any trouble breathing, speaking, or swallowing? Do they feel weaker than usual in the arms or legs? You don’t need a full neurological exam, but you do need a clear impression.
When to refer for urgent medical attention
Often, the patient's energy and general demeanour offer clues. A bright, alert patient with mild lid droop but no other symptoms probably isn’t experiencing a medical emergency. Still, document everything clearly. Reassure, but don’t dismiss their concern.
If your patient reports symptoms such as blurred vision or struggling to keep their head upright. Should you notice their speech is at all slurred, or breathing feels shallow, that’s when you move to an urgent A&E referral.
This referral is about protecting the airway and monitoring for progressive paralysis. It’s rare, but your threshold for action should be low.
There’s a grey area, of course. Occasionally, patients may present with anxiety or health fears that mimic more serious symptoms. That doesn’t mean their experience isn’t real. But it does mean your role is part-clinician, part-investigator. Listen carefully and don’t rush to judgement.
Documentation matters here. If you suspect botulism, refer and record. If you’re confident it’s cosmetic ptosis, still note onset, severity, and your reasoning. This helps with continuity and protects you if symptoms change.
Botulism cases from cosmetic botox are extremely rare
It’s important to remember, botulism cases related to cosmetic botulinum toxin are extremely rare. Plus, most documented incidents involve counterfeit botox. Still, we understand that the fear can be real for patients. Occasionally this can also be true for practitioners, too, especially when your patient presents unusually.
Use your clinical judgement and consider asking colleagues for their input. Ultimately though, when in doubt, refer. It’s never wrong to escalate if you’re unsure. Better a patient gets checked and reassured than missed at the wrong moment. As an aesthetic practitioner, you’re not a neurologist but you are responsible for your patient’s safety.
Knowing the difference between ptosis and botulism, and knowing when to act, is what separates technical skill from clinical leadership.
As a medical professional, you’ll have honed your skills in relation to staying calm and methodical. Your aesthetics training should then build on this, to ensure you do everything you can to minimise the likelihood of complications, but are fully prepared to manage them, should they occur.
Because being a good injector isn’t just about where you put the needle. It’s about what you notice afterwards and how you respond when things don’t go as planned.
All information correct at time of publication
Download our full prospectus
Browse all our injectables, dermal fillers and cosmetic dermatology courses in one document
By submitting this form, you agree to receive marketing about our products, events, promotions and exclusive content. Consent is not a condition of purchase, and no purchase is necessary. Message frequency varies. View our Privacy Policy and Terms & Conditions
Attend our FREE open evening
If you're not sure which course is right for you, let us help
Join us online or in-person at our free open evening to learn more
Our Partners













STAY INFORMED
Sign up to receive industry news, careers advice, special offers and information on Harley Academy courses and services


