Koebner Phenomenon: What Aesthetics Practitioners Need to Know

An interesting case in the UK has sparked discussion about injectables and the Koebner phenomenon. But what exactly is it?
In this article we explore what aesthetic practitioners need to know about the Koebner phenomenon and its links to cosmetic injectables.
Read on to educate yourself about this issue and the British man who developed acute psoriasis following filler treatments.
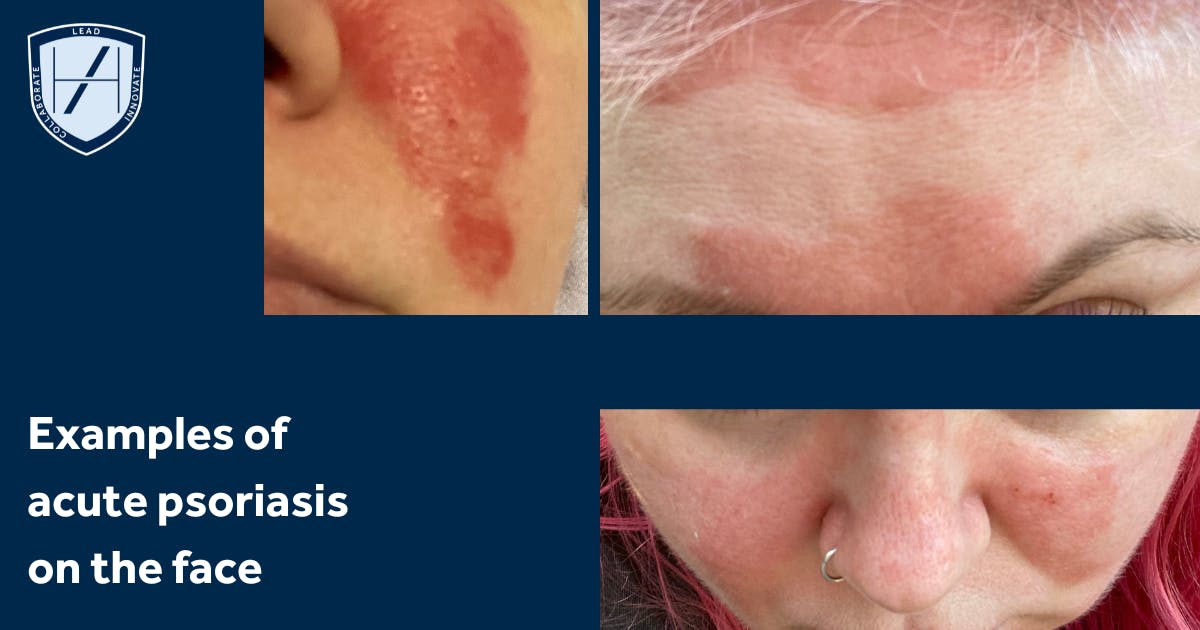
Examples of a patient who developed widespread acute psoriasis following a tattoo
What is the Koebner phenomenon?
The Koebner phenomenon describes new lesions of a skin disease appearing in areas of skin that were previously unaffected, after some form of trauma or injury. It also refers to the triggering of an active skin disease where the patient had an underlying predisposition.
This ‘trauma or injury’ is broad in scope and includes:
- Cuts or scrapes
- Burns, including sunburn
- Insect stings
- Tattoos
- Surgical incisions
- Injections.
Research has found that people may fluctuate between ‘Koebner-positive’ and ‘Koebner-negative’, making it highly unpredictable.
Mechanistically, the exact cause isn’t fully known. Hypotheses include release of inflammatory mediators, activation of tissue-resident memory T cells, nerve growth factor, vascular changes, and disrupted keratinocyte behaviour.
Reverse Koebner and Wolf’s isotopic response
Where this issue triggers lesions, ‘reverse Koebner phenomenon’ causes existing skin lesions to disappear following trauma.
It’s useful to understand the difference between Koebner and Wolf’s isotopic response, given the two appear similar. Both can induce new skin lesions in previously unaffected skin following trauma. However, Wolf’s involves lesions being present beforehand and a more generalised skin disease response after.
Which skin conditions can be triggered by the Koebner phenomenon?
The skin conditions this typically refers to are:
- Psoriasis, most commonly
- Vitiligo
- Lichen planus.
It’s reported that around 25% of patients with psoriasis may develop a Koebner-type response to skin injury.
Koebner phenomenon effect on injectable patients
Given it can be triggered by breaking the skin, as an aesthetic practitioner, it’s important to understand the Koebner phenomenon.
In the context of aesthetic practice, although fillers, botulinum toxin and other cosmetic injectables, or, more specifically their injection trauma, haven’t been extensively studied for Koebner risk, the risk is plausible.
Examples of published data include a 2015 published case report on glabellar botox triggering skin lesions in a patient with a history of psoriasis. The authors concluded that the cutaneous needle trauma prompted this, not the neurotoxin itself.
Another review of the Koebner phenomenon in psoriasis from 2019 describes the potential for new lesions following tattoos, piercings, burns, surgical incisions and even pressure or swelling.
British man developed acute psoriasis following filler treatments
In January 2025, a teenage author from Lancashire spoke about being diagnosed with the “worst case of psoriasis doctors have ever seen”. He tied this to receiving 18 filler treatments within a 3-month period as part of social media influencer agreement.
He campaigned for pre-filler patch tests to be made mandatory, saying, “There should be a law in place to protect people like me.”
The 18-year old conceded that an underlying propensity for psoriasis may lie dormant until activated. However, it appeared it had not been explained to him that his response was likely due to a predisposition being triggered by the physical injection via the Koebner mechanism, rather than the filler product.
Three factors for assessing patient risk
There are three key factors to consider when assessing a patient’s Koebner risk:
- Whether they have a known predisposition, such as psoriasis or a history of psoriatic lesions
- Needle or cannula insertion, placement of your gel or toxin, swelling and/or pressure from this procedure may cause trauma to the injected area and/or adjacent skin
- If the disease is in a more reactive state, such as active, unstable skin or where your patient has had a recent flare.
Where these align, your patient may have a higher risk but outcomes are highly unpredictable.
So what does this mean for you as an aesthetic practitioner? Essentially, you should be aware of this phenomenon and its potential impact on specific cohorts. But it doesn’t automatically preclude treatment.
Be aware that injection sites may respond differently
It’s important to understand that injection sites might behave differently in aesthetic patients with a Koebner-positive skin history.
You may see new psoriatic lesions at the filler site or nearby, a flare of psoriasis, or more inflammatory reactions. There may also be more heightened responses after treatment, such as bruising, swelling, and delayed healing.
Again, the risk is not uniform nor guaranteed. Many patients with psoriasis undergo aesthetic treatments without Koebner responses.
Decide if you’re comfortable treating where this risk is present
Whether you warn relevant patients about their potential for Koebner response is an ethical decision each aesthetic practitioner should make for themselves.
It can be useful to consider if you’re confident in treating patients with this risk profile. Especially if you’re a novice injector, perhaps you’ve completed Foundation Training in Medical Aesthetics so have a basic grounding, but lack solid clinical experience.
As a beginner, your clinical judgement and reasoning will not be as informed, so it’s normal to want to wait until you’re ready before tackling potentially complex cases.
Screen your patients ahead of an appointment
It’s often wise to ask patients to answer a few basic screening questions before an appointment. You can include a question that alerts you to Koebner possibility, such as ‘Do you now or have you ever had psoriasis, vitiligo or lichen planus?’
This gives you room to follow up for more information to determine if a consultation is worthwhile. Alternatively, you may opt not to treat based on the information provided.
Being able to review patients in advance can avoid time wasting for both parties. It can also prevent uncomfortable conversations in person, although there’s no better learning curve than experiencing these situations and having to deal with them, in real time, face-to-face!
Prepare prompts for follow-up and refusing treatment
It can be helpful to prepare a short script or set of prompts that you can use in this scenario. For example, noting that you:
- Have reviewed the information they’ve kindly provided
- Noticed a potential contraindication for treatment
- Would like to have a quick chat about this; or
- Are sorry to say that you will not be able to treat them as a result of this, and give a brief explanation as to why.
If possible, offer to refer them to another practitioner with more experience in these cases. Don’t let the fear of losing out on potential business prevent you from providing the best possible service, especially if you’re not in a position to help them at present.
Even if you never see that patient again, their having had a good and ethical experience can still generate great word-of-mouth referrals!
Adapting your clinical consultation for higher-risk patients
If you do decide to go ahead with the consultation, you may need to allow more time for a more detailed clinical consultation. This will allow you to get a fully-rounded view before making any decisions regarding treatment.
How to adjust your consultation for potentially higher-risk patients
If your patient reports any psoriatic history, lichen planus, vitiligo or related dermatoses, you should include all the usual consultation elements, but can explore this particular facet further in the following ways…
1. Take a more detailed medical history
Ask your patient about
- Disease activity, including recent flares and stability
- Sites of previous plaques, In the case of psoriasis
- Current treatment for this condition, eg. topical, systemic biologics, or immunosuppressants
- Previous experience of skin trauma leading to lesions, such as tattoos, piercings or burns
- Whether they know if they exhibit a Koebner response
- Pre-existing dermatoses and whether they’ve been told they are “Koebner positive”.
2. Assess your patient’s skin
- Examine the skin both within and near the treatment area
- Look for active plaques, recent lesions, and signs of inflammation
- Evaluate their skin integrity, vascular supply, and whether the skin is stable or fragile
- Review the proposed injection area for skin health, signs of recent trauma, plaque or thickening nearby.
3. Consider their risk profile and discuss this
Although we know Koebner is wildly unpredictable, we can determine potential risk.
- Potentially low risk: Stable condition, no recent flares, treatment maintained, and healthy skin in the treatment area, risk may be lower
- Likely high risk: Active or poorly controlled condition, or where the treatment area is compromised.
Once you’ve assessed this, you can take your patient through it, making sure you use accessible language that doesn’t cause undue alarm.
- Give them a brief explanation as to what the Koebner phenomenon is, including its unpredictability
- Note that, although the data is limited, there’s a plausible risk of new lesions via the Koebner mechanism
- Explain that this is due to injections being a potential trigger
- Discuss the anatomical area, including how injecting a previously unaffected region may increase their theoretical risk of sparking a flare at or around the injection sites.
Steps for proceeding with treatment
If you decide you’re happy to proceed with treatment, be mindful of setting realistic expectations. The aesthetic outcome may be pleasing, but should a Koebner response occur, dermatological treatment may be required.
Ensure your patient understands the process and has all the relevant details for aftercare, follow-ups and any out-of-hours emergencies.
If you’re unsure about the their dermatological status, consider liaising with their dermatologist. You could also recommend a dermatology review prior to taking a decision about treatment. This is a solid pathway should the patient be on systemic biologics or have unstable disease.
Informed consent and documentation
For medicolegal reasons, record all discussions and assessments in your patient file. These are key to the informed consent process and should be documented meticulously.
Also align your documentation to your indemnity insurance provider’s requirements.
As a guide, your file notes should include:
- The patient’s disease history
- Level of control
- That you explained the Koebner phenomenon to them and they confirmed they understood
- The risks and potential outcomes post-treatment that you advised them of, and which they confirmed were understood
- Any aspects they were concerned about and your responses
- Details of the mutually agreed treatment and management plan
- What, if any, reference material was provided to the patient in relation to pre- and post-procedural care, as well as emergency situations
- Any steps or adjustments you advised you’d make to help minimise trauma particularly during injection.
Injection technique adjustments for patients with a Koebner risk
You may wish to consider:
- Using the ‘low and slow’ approach - injecting low volumes, slowly, using a gentle pressure
- Choosing injection sites with lower risk, avoiding areas with recent trauma or inflammation
- Ensuring your patient’s skin is in optimal condition prior to treatment
- Pre- and post-care to reduce inflammation.
Lastly, closely monitor the patient throughout the treatment.
We hope this article has taught you something new and would love to know how you feel about treating this cohort. Do you feel ready? Let us know via the Harley Academy Instagram account!
All information correct at time of publication
Download our full prospectus
Browse all our injectables, dermal fillers and cosmetic dermatology courses in one document
By submitting this form, you agree to receive marketing about our products, events, promotions and exclusive content. Consent is not a condition of purchase, and no purchase is necessary. Message frequency varies. View our Privacy Policy and Terms & Conditions
Attend our FREE open evening
If you're not sure which course is right for you, let us help
Join us online or in-person at our free open evening to learn more
Our Partners













STAY INFORMED
Sign up to receive industry news, careers advice, special offers and information on Harley Academy courses and services


